Looking At The Gut And The Ecosystem Inside It
Gastroenterology is not a new field of study, but scientists, pharmas and clinics around the globe have only recently started realising just how significant it is to our health. Partly, this has to do with an increasing interest in how our diet can influence our fitness, weight and longevity - given that it's our gastrointestinal system that processes all of what we consume - but it also has to do with recent advances in technology used in DNA sequencing and automated cell culturing, allowing researchers to more thoroughly explore the multitudes of cells in our gut.
The gut is a miraculous organ, I think, and most gastroenterologists will probably think the same (they make a living from it, after all!). Some, I hear, even proclaim it to be as complex and important as our brain, which is an interesting comparison. Though I'm not sure whether to agree with it, it is a fact that, like our brain, we still have yet to discover all the functions that make up our digestive system. There are the basic functions of breaking down, absorbing and excreting what we consume, of course, but those only comprise part of its complexity.
In this post, we'll be looking at some of the more subtle parts of the bacterial ecosystem that lives in our gut. To begin with, however, we must first come to terms with the basic anatomy that supports it.
The Gastrointestinal System
We begin with the mouth. Here, teeth chew through large chunks of solid food to increase their surface area for when they enter the stomach below. This process - known as mechanical digestion - is complemented by constant secretions of saliva produced in salivary glands through four nodes in our mouth. Saliva contains amylase enzymes that digest large starchy carbohydrates in the food, with sticky mucein proteins that help in trapping bacteria and joining small bits of food together to then form boluses. The saliva lubricates these as they are swallowed, at which point involuntary muscular contractions and relaxations in the oesophagus systematically force them down (a process known as peristalsis).

Once a bolus enters the stomach, the pyloric sphincter, which acts as the entrance to the small intestine, closes. And it refuses to budge for a good long while, letting the bolus soak in the stomach's gastric acids as proteins get digested by peptidases. Finally, after maybe two hours or so, the pylorus opens and lets the softened chyme into the first part of the small intestine - the duodenum.
In the duodenum, digestive enzymes and bile (from the pancreas and gallbladder respectively) are secreted by cells lining the intestine's walls. These help fully digest the chyme, flowing alongside it into the jejunum and ileum. These are the longest stretches of the small intestine by far, with folds in the wall's lining (i.e vili) increasing its surface area for absorption of nutrients and water. Any unabsorbed, insoluble material then heads into the ascending colon, where more water is absorbed from the chyme to solidify it into faeces. This is moved into the descending colon and the rectum to be stored until it can finally be excreted out of the anus. (Do note that, when you are properly hydrated, less water is reabsorbed in the colon to soften the faeces for easier egestion. Always make sure to drink lots of water!)
And that's the basics of the digestive system - the most discernible parts, even. But where do the tonsils come in? Or the appendix, so sadly popularised as a useless grass grinder for so long? And the gut bacteria - what's up with those?
Let's find out.
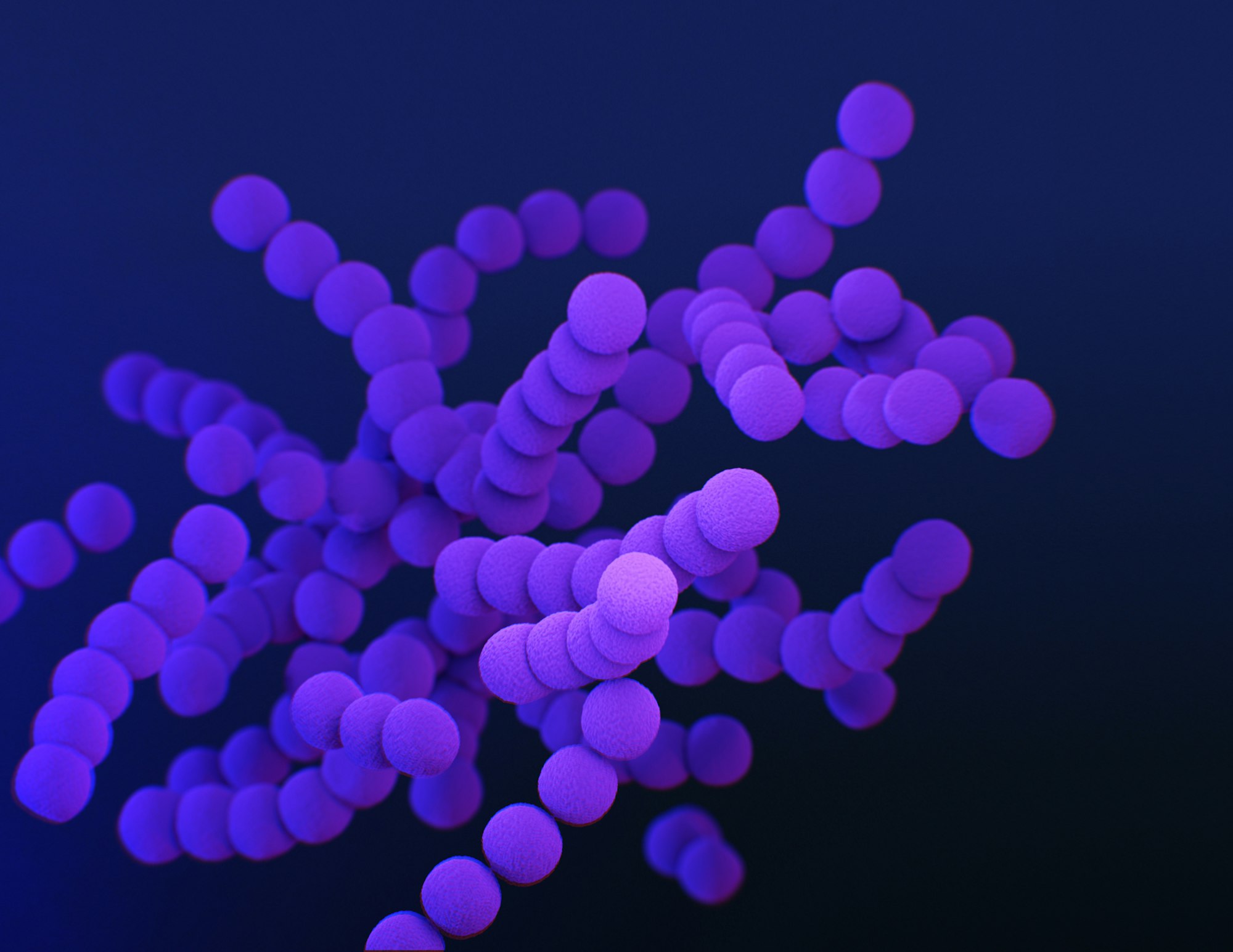
The Gut Microbiome
Ever since Robert Koch discovered the bacteria responsible for tuberculosis and cholera in 1882-1883 (which won him a Nobel prize!), the field of bacteriology has exploded in popularity. Any reputable pathologists and hospitals nowadays will have sectors dedicated to treating bacterial infections, with the topic widely included as a principal course of study in school biology. As such, it should come as no surprise that bacteria are being researched day in and day out by essentially every influencial country in the world - with much progress being made in researching our own gut bacteria.
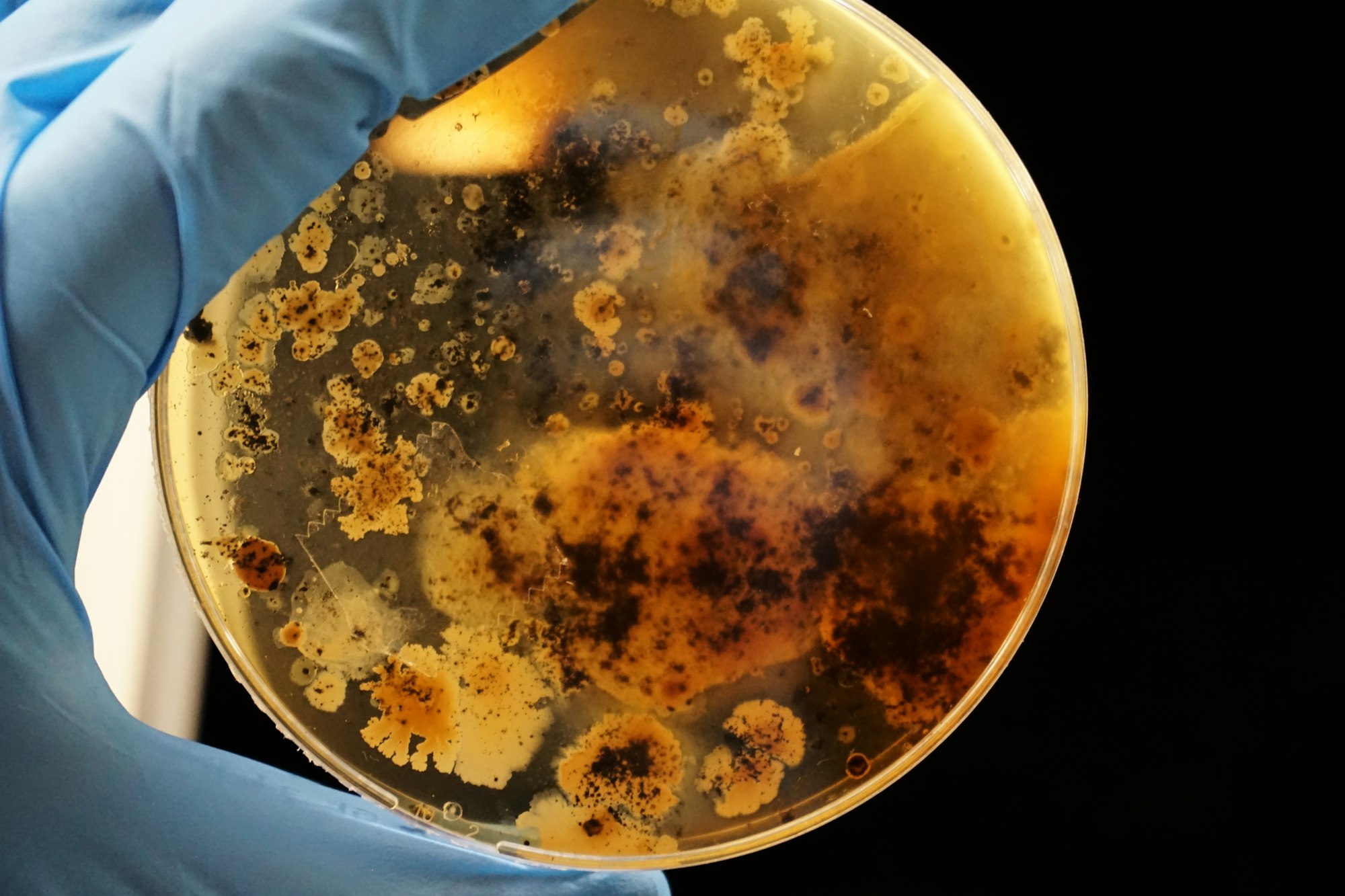
Most people, I find, think of the majority of bacteria as harmful, virulent creatures that cause disease wherever they go. For the most part, this is not true; less than 1 percent of bacteria make people sick, and most species simply go on with their lives without affecting us in the slightest. This is doubly true in the case of our gut flora (which is just a fancy name for the microbiome in our gut), as, under normal circumstances, microbes there are strictly regulated by our immune system. White blood cells routinely enter out intestinal tract and search for harmful invaders, killing them as soon as they are spotted; the rest are left alone. Theories for how white blood cells can tell different microbes apart like that are still being developed, but a popular one is that the microbiome itself trains our immune system to recognise pathogens and make them used to typical inhabitants that they shouldn't kill. (If you are interested, recent studies on this found the specific proteins that some gut bacteria can use to stimulate an immune response in mice, called immunostimulatory muropeptides.)
Our tonsils and appendix are lined with immune tissue and have a high concentration of white blood cells, and these places play a significant role in training our immune system for accurate pathogen detection (particularly in children). Apparently, the appendix further acts as a storage of good bacteria to repopulate our gut flora after we've been infected by pathogens or have otherwise had issues in our gut.
What are good bacteria, though? Essentially, these are species that live in a mutualistic relationship with us (such as the symbiosis between some luminescent bacteria and squids), which feed off undigested molecules in the colon and produce vitamins, hormones and other molecules that are beneficial to us. Bacteria living in our gut are also useful to prevent other, disease-causing species from colonising the space and outcompeting/bullying the good bacteria into oblivion. Again, the appendix storage helps prevent this, too.
Alas, just as our gut flora can help us if we maintain it well, it can damage us if we disregard it completely; like a garden, we must cultivate it caringly and uproot the weeds that pop up unnoticed.
IBS & A Leaky Gut
For the past couple of months, my mother has been dealing with a condition known as irritable bowel syndrome (IBS). She experiences stomach aches, inflammation in her bowel and in her right foot, and other irritations. 'What does her right foot have to do with her bowels?' you might ask. I'll attempt to answer that in a moment. Though my mother would perhaps disagree with me given her experience in the matter, to me, the subject of IBS and other such gut disorders is actually an incredibly interesting field of study, with much potential for improvement in the future. As such, here's a summary of the basics of IBS.
Belonging in a category for bowel disorders referred to as disorders of brain-gut interaction (DGBIs), IBS is a condition caused by an imbalance of one's gut flora that incduces stress signalling between the brain and the gut and produces irritation. This occurs when some species of bacteria have grown in number and overtaken other, less dominant strains in their intestinal ecosystem, which is caused by an improperly balanced diet. For instance, when you consume too many sweeteners for long periods of time (which your body can't digest), these end up in the colon and incite an increase in the number of bacteria in the bacteroides genus - while causing a decrease in the clostridiales genus. Ultimately, researchers have found, this can promote insulin resistance and glucose intolerance, thereby increasing your risk of obesity (which means that too many sweeteners do make you fat, albeit indirectly). Bacteroides and other such species are also responsible for stomach gases, causing bowel inflammation.
In regards to my mother's foot - I believe it might be a consequence of leaky gut syndrome (which is a a rather strange name for a medical condition). This is when our gut lining becomes more permeable as a consequence of prolonged periods of stress, gluten intolerance and, probably, IBS. Toxins and unwanted bacteria can then enter the blood stream through your gut, triggering an immune response and causing inflammation in the most random places on your body - which can be very painful. Fortunately, if you are experiencing this, there are ways of getting better. In order to alleviate the symptoms and to improve the condition in general, I recommend visiting a good nutritionist to alter your diet and make it specific to your situation - though eating fewer sweets, sweeteners and junk food is a good way to start. Furthermore, consuming prebiotics (high-fiber food that is beneficial to good gut bacteria, such as asparagus or leek) and probiotics (food that contains good bacteria by themselves, like yoghurt) would probably help in the process. (A disclaimer: I am neither a gastroenterologist nor nutritionist, and all of my advice is informal in nature. Please visit a professional if you feel that you would benefit from medical assistance.)

Like the immune system (which I wrote about in a previous post), there is much research to do on the gut flora and DGBIs, as we have yet to truly understand the full extent of their mechanisms. If you want to read more about it, however, I recommend 'Gut', by Giulia Enders; it is a lovely book, and acted as one of the inspirations behind this post.
References
- Arnold, J. W. (2016). Emerging Technologies for Gut Microbiome Research. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5074899/
- NIH (n.d.). Bacterial Infections. Agency for Healthcare Research and Quality. Retrieved from https://effectivehealthcare.ahrq.gov/health-topics/bacterial-infections
- Blevins, S. M. & Bronze, M. S. (2010). Robert Koch and the ‘golden age’ of bacteriology. ScienceDirect. Retrieved from https://www.sciencedirect.com/science/article/pii/S1201971210023143
- Ansaldo, E. & Belkaid, Y. (2021). How microbiota improve immunotherapy. Science Magazine. Retrieved from https://www.science.org/doi/abs/10.1126/science.abl3656
- Cheriyedath, S. (2019). Why do humans have an Appendix? News-medical. Retrieved from https://www.news-medical.net/health/Why-do-Humans-have-an-Appendix.aspx
- Suez, J. et al (2014). Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25231862/
- Sethi, S. (2019). What to know about leaky gut syndrome. Medical News Today. Retrieved from https://www.medicalnewstoday.com/articles/326117
- Enders, G. (2014). Gut: The Inside Story of Our Body's Most Underrated Organ. Scribe Publications.
