Prion Proteins & The Deadly Diseases Associated With Them

A pathogen does not need to be alive to cause infection. In fact, a very large percentage of the most dangerous and frightening diseases we know of are caused by such pathogens. But we have seen this before. Though there is a divide in opinions, for example, most biologists think of viruses as non-living particles (albeit rather complex ones) due to their inability to reproduce or metabolise without a host. In other words, this means that conditions like polio, AIDS, common colds and other such virus-caused diseases are all inherently caused by non-organisms - but only technically. Even viruses must rely directly on genetic material (i.e., DNA and RNA strands) to propagate themselves, as they encode instructions for the proteins that make them inside their host cells. As such, it might seem that the first statement is really only a technicality. And then you discover that viruses are only the start.
Let me introduce you to the humble prion. If sentience could be measured in objects both alive and inanimate, prions would be hitting a stage almost as low as rocks in the chart (that is to say, very low). This is because prions are actually just specific types of proteins, with the word 'prion' literally obtained from combining the nouns 'protein' and 'infection' together. (Clever, eh?) Like the name suggests, these are characterised by their distinct capability of infecting organisms by themselves and can therefore act as infectious pathogens inside us - and most of the time they do so both incredibly quickly and inexorably, with most of associated cases ending with life-altering complications or just straight-up death. Once they have spread and propogated, they can also become almost unstoppably contagious; much more, in fact, than even our dear pandemic-starter, Dr 'Rona.
Luckily for us, prion diseases are very rare in humans, and most of the time can be detected and tracked quickly enough to prevent uncontrolled spread through the population. It is so rare, in fact, that epidemiologic studies by the CDC on the issue find that only about 1 in 6,000 people get a prion disease in their lifetime (in the US, anyway). This number varies with different populations around the world, but, in general, you can be assured that you very probably won't get one. Be adviced, however. If you do contract a prion, you better get to the hospital like your life depends on it - because it very probably does.
A Spread Of Deconstruction
Before taking notice of their effect on humans, prion diseases were first observed in Merino sheep in 19th century Spain. The condition at the time was often fatal, and shepherds frequently observed their sheep scraping against fences before the disease took them. Prions had not yet been identified at the time (though proteins had), and so this condition was named simply for its effects on behaviour; it was termed scrapie.

Around the time that scientists started realising that the agent for scrapie was a protein (credit to Stanley B. Prusiner, who won the Nobel Prize in Physiology or Medicine in 1997), they also became strangely interested in British cows. With the outbreak of a condition termed 'Mad Cow Disease' in the UK in 1985 (which negatively affected the behaviour in cows), this meant that researchers could propose a connection between it and scrapie. Now known more objectively as bovine spongiform encephalopathy (BSE), the condition was the beginning of our scientific studies on infectious proteins in the brain, and has since become a role-model for prion diseases in general.
Together with scrapie, BSE was later allocated to a group of related prion diseases referred to as transmissible spongiform encephalopathies (TSEs). The name, of course, comes from the sponge-like shape and appearance of the brain after infection (which I think would probably look more terrifying than it sounds). In regards to BSE, scientists soon discovered that the condition slowly degrades the functional proteins in a cow's brains, thereby causing brain cells to essentially kill themselves and deattach from the surrounding tissue matrix. The result: a gooey soup of infected cow brain. (Honestly, though, how terrifying could it be?)
Most prion diseases found in mammals (including scrapie and BSE) are caused by an aberrant misfolding of a lucrative and imaginatively named prion - the prion protein (PrP). PrP has two forms: either it is made up of a number of alpha-helix amino acid sequences joined together, as normally apparent in cells and known as PrPC; or it is altered to have a higher quantity of amino acid beta-sheets that make the protein insoluble and damaging to the cell, turning it into PrPSc. (The 'Sc' just comes from the term 'scrapie'.)
The mechanisms by which PrPC can turn into PrPSc are widely debated, but most predict that it can arise from a variety of sources. These include gene mutations in the prion protein gene, PRNP; externally acquired infections from other individuals with the condition; and even simple spontaneity, with random chance and bad luck making PrPC fold inside the body in just the right way to become PrPSc. And that is exactly what happened to one of those poor cows with BSE.
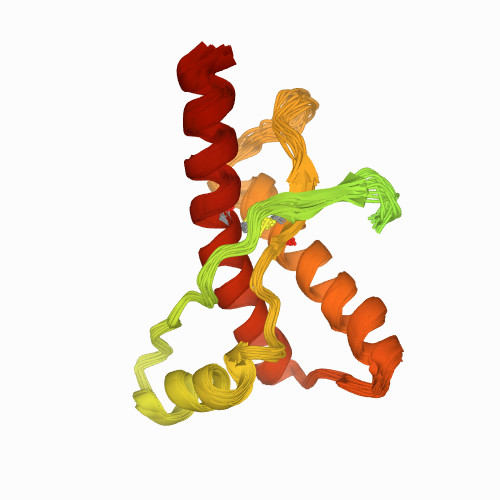
Unlike viruses, a PrPSc does not need to affect the host's DNA to propagate itself. Instead, it does so very directly by acting on the PrP proteins surrounding it, catalysing a reaction that alters them into prions themselves. In turn, the transformed prions can act on other PrPCs in the cell, which are transformed and act on other proteins, and so the cycle turns and exponentially affects body cells and health.
Normally, PrPC has the role of preventing cells from commiting programmed cell death (called apoptosis) and slowing down oxidative damage to the machinery that runs the cell inside. It is also partially responsible for holding cells together, keeping them from moving away from their regular position in the cell tissue. As such, we can see why the spread of PrPSc - which is faulty and cannot operate any of the typical functions of its healthy variant - can lead to groups of neural cells in the brain dying and causing the giant disturbances observed in cows plagued by BSE. This is the essence of prion diseases - they lead to mass organ failure in the body, particularly affecting the brain. In humans, prions act very similarly as in sheep and cows, and so we too have our own TSEs to look out for. Creutzfeldt-jakob disease and Gerstmann-Straussler-Scheinker syndrome are two of them, and neither is very pretty. How they arise in people is variable and still under investigation, but there are some proven trends behind them that we know of.
Like with BSE, human TSEs are known to come from one's genetic heritage and random PrP missfolding. Some of the time, people can take precaution from acquiring TSEs, especially if they have had their DNA sequenced and know how at risk they are. Unfortunately, however, studies have found spontaneous misfolding to be the most common cause of prion infections in humans, with about 85 percent of annual cases occurring from it. Since prion diseases tend to remain docile for months or even years before they start producing symptoms, this means that people often remain unaware of their infection until the clinical stage. At this point, prion diseases can become so rampant that, sadly, it can take only weeks before they become terminal.
What about our immune system, though? Why couldn't it just eliminate prions, just as it does with the numerous other pathogens that invade our bodies within our lifetimes?
Immune Faults & Prion Vaccines
Though our immune system is frankly incredible at obliterating most pathogens (as we have seen before), researchers have found it to be startingly lax when dealing with prions. Since researchers began looking for prions in the 1970s, they have not found a single coordinated immune response that targeted prions in the body of any animal. Several researchers claim that it is due to a lack of differentiation of missfolded prions from regular ones, preventing immune cells from reacting to them. Others suggest that it is actually the uncanny ability of PrPSc to resist protein degradation by white blood cells. Should this be the case, antigen-presenting white blood cells would be unable to break down PrPSc, thereby preventing them from stimulating other immune cells from producing antibodies and essentially blocking the whole response at the very start.
To circumvent this issue, researchers are trying to find ways to start the immune response against prions mannually. With sufficient tinkering and chemical synthesis in the lab to find novel biomolecular compounds that are safe to use (which might be assisted by accelerated discovery), we may eventually find immunological stimulants to treat prion diseases - which may be sort of like a prion vaccine, if you will.

Prion diseases like TSEs are very rare in our community, being seen in only one in thousands around the world. When you sum up global cases in the population, however, the numbers become significant. Thousands of people get TSEs per year - and the annual cases are only increasing with time. They are also particularly perilous when contracted, being fatal in most victims when left unchecked (and even cannot be cured for certain when detected). As such, it is no wonder that so many medical researchers are fervishly working to find treatments for prion diseases nowadays. As with all pathological fields of study, however, I believe that current progress will one day make even prions an obsolete worry of the past. They are only molecules, after all!
References
- CDC (2021). Prion Diseases. CDC. Retrieved from https://www.cdc.gov/prions/index.html
- Minikel, E. V., et al (2019). Age at onset in genetic prion disease and the design of preventive clinical trials. Neurology 93(2). Retrieved from https://doi.org/10.1212/WNL.0000000000007745
- Zabel, M. D. & Reid, C. (2015). A brief history of prions. Pathogens and Disease 73(9):ftv087. Retrieved from https://doi.org/10.1093/femspd/ftv087
- Sigurdson, C. J., Bartz, J. C. & Glatzel M (2019). Cellular and Molecular Mechanisms of Prion Disease. Annual Review of Pathology 14:497-516. Retrieved from https://doi.org/10.1146/annurev-pathmechdis-012418-013109
- Eghiaian, F., et al (2004). Insight into the PrPC-->PrPSc conversion from the structures of antibody-bound ovine prion scrapie-susceptibility variants. Proc Natl Acad Sci USA 101(28):10254-9. Retrieved from https://doi.org/10.1073/pnas.0400014101
- Zabel, M. D. & Avery, A. C. (2015). Prions--not your immunologist's pathogen. PLoS pathogens 11(2):e1004624. Retrieved from https://doi.org/10.1371/journal.ppat.1004624
- Legname, G. & Moda, F. (2017). The Prion Concept and Synthetic Prions. Progress in Molecular Biology and Translational Science 150:147-156. Retrieved from https://doi.org/10.1016/bs.pmbts.2017.06.002
